Polyethylene glycol (PEG), as a pharmaceutical excipient, is widely used in drug formulation development and production due to its good biocompatibility, water solubility, and tunable physicochemical properties. Its core functions revolve around improving drug performance, optimizing formulation quality, and enhancing therapeutic efficacy, which can be categorized into the following areas:
I. Improving Drug Physicochemical Properties and Enhancing Formulation Applicability
(I) Increasing Drug Solubility and Dissolution
Some drugs exhibit poor water solubility, leading to slow dissolution after oral administration, low bioavailability, and difficulty in reaching effective therapeutic concentrations. PEG can enhance a drug's solubility in water by forming hydrogen bonds with drug molecules, encapsulating drug molecules, or altering the drug's crystal structure. Concurrently, its good water solubility promotes uniform dispersion of the drug within the formulation and accelerates the drug dissolution rate, making the drug more readily absorbed by the body. This is suitable for solubilizing and aiding the dissolution of poorly soluble drugs in oral solid dosage forms (e.g., tablets, capsules).
(II) Enhancing Drug Stability
Drugs are susceptible to degradation, oxidation, or polymorphic transformation during storage or preparation due to factors such as temperature, humidity, and light, leading to reduced efficacy or impurity formation. PEG can form a protective film on the surface of drug molecules, shielding them from environmental influences. Simultaneously, its molecular structure can inhibit crystal growth or polymorphic transformation of the drug, maintaining its stable form. Furthermore, in liquid formulations, PEG can act as a stabilizer, preventing agglomeration or precipitation of drug particles, thereby ensuring the formulation's performance stability throughout its shelf life.
II. Optimizing Formulation Performance to Meet Different Administration Needs
(I) Modifying the Formability and Mechanical Properties of Solid Dosage Forms
In the preparation of oral solid dosage forms (e.g., tablets, granules), PEG can serve as a binder or lubricant. As a binder, it enhances cohesion between drug powders, resulting in granules with good flowability and compressibility, facilitating tablet formation and reducing issues like tablet capping or lamination. As a lubricant, it reduces friction between drug particles and the die, as well as internal friction within the granules, improving tablet surface smoothness, minimizing sticking during compression, and enhancing production efficiency.
(II) Improving the Texture and User Experience of Semi-Solid Formulations
In semi-solid formulations such as ointments, creams, and gels, PEG can function as a base or thickener. As a base, it uniformly mixes with other excipients (e.g., oils, active ingredients), forming a smooth, stable ointment or gel with good spreadability for even application on skin or mucosal surfaces. As a thickener, it adjusts the formulation's viscosity, preventing separation or runoff due to insufficient viscosity, while also improving skin feel during application, reducing greasiness, and enhancing patient compliance.
(III) Facilitating the Preparation and Functionality of Sustained- and Controlled-Release Formulations
Sustained- and controlled-release formulations aim to achieve stable blood drug concentrations, prolong drug action, or reduce dosing frequency by controlling the drug release rate. PEG can serve as a sustained-/controlled-release material in the preparation of matrix-type, membrane-controlled, and other such formulations. In matrix-type formulations, PEG can form a three-dimensional network structure that encapsulates drug molecules, allowing for slow release through matrix erosion or drug diffusion. In membrane-controlled formulations, it can be a component of the coating material, modulating the permeability of the coating membrane to control drug release rate, enabling drug release at a predetermined rate to meet clinical needs for long-acting therapy.
III. Enhancing Medication Safety and Biocompatibility
(I) Reducing Drug Irritation
Some drugs can irritate the gastrointestinal mucosa or injection sites, easily causing discomfort (e.g., nausea, vomiting, local pain) after oral or injection administration. PEG can reduce direct contact between the drug and the mucosa by encapsulating drug molecules. Its mild physicochemical properties can also buffer the drug's irritation to local tissues, lowering the incidence of adverse drug reactions. For instance, in injectables, PEG can act as a co-solvent and stabilizer, not only improving drug solubility but also reducing irritation at the injection site, thereby enhancing medication safety.
(II) Ensuring Formulation Biocompatibility
As a pharmaceutical excipient, PEG must possess good biocompatibility to avoid triggering immune reactions or toxic effects in the body. Its simple molecular structure lacks allergenic groups, and it can be excreted through urine or feces in the body, with minimal tendency to accumulate in tissues, thus having little impact on normal physiological functions. Therefore, when used in formulations for various routes of administration (e.g., oral, injection, topical), it helps ensure formulation safety and reduce excipient-related adverse reactions.
IV. Assisting in the Preparation and Functionality of Special Formulations
(I) Acting as a Co-Solvent and Stabilizer in Injectables
In injectables, some drugs are difficult to formulate into clear solutions meeting requirements due to low solubility or poor stability. PEG can serve as a co-solvent, enhancing the drug's solubility in water for injection, helping the formulation achieve a clear, transparent standard. Simultaneously, it can inhibit drug degradation or aggregation during storage, maintaining the stability of the injectable and ensuring drug efficacy and safety during use.
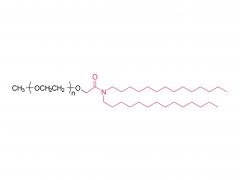
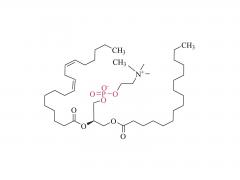
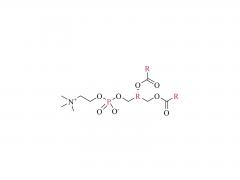
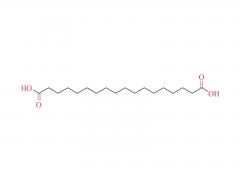
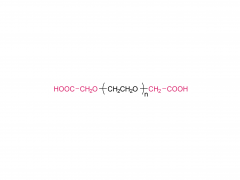
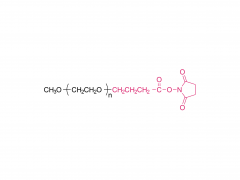
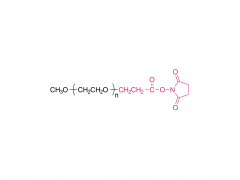
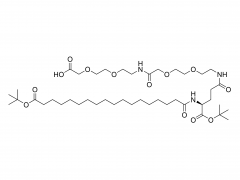
(II) Use in Carrier Modification for Targeted Formulations
In targeted drug delivery systems (e.g., liposomes, nanoparticles), PEG can serve as a carrier surface modification material. By attaching PEG chains to the carrier surface, it can reduce the likelihood of the carrier being recognized and cleared by the mononuclear phagocyte system in vivo, prolonging its circulation time in the bloodstream and creating conditions for the drug to reach the target site. Furthermore, its surface can be further modified with targeting ligands to enhance carrier specificity, enabling the drug to act more precisely on the lesion site and reducing damage to normal tissues.